In the past couple of decades, America has seen a doubling of patients for Diabetes, accounting for almost 38 million adults in the country’s population. Youth, however, do not escape diabetes either. Teens like Jennifer Guerrero (12), Siri Larsen (11) and Margaret Hatley (9) have to carry the weight that comes with diabetes while dealing with the stresses that come with school work and life.
All three of these White Station students were diagnosed with type one diabetes. Type one is when the pancreas stops producing the cells that make insulin – a hormone that regulates blood sugar levels. Type two deviates from this in the way that people with it are insulin-resistant. However, contrary to popular belief, there are other, less commonly known types of diabetes that affect a smaller portion of the population.
“Type two diabetics … create insulin,” Larsen said. “They’re just resistant to their own insulin. And type 1 diabetics don’t make it at all. So oftentimes, type one diabetics will be diagnosed when they’re hospitalized because their blood sugar is so high because they don’t create the insulin.”
Luckily for him and his peers, Gurrero and Hatley, they did not become hospitalized before they were diagnosed. All three of them experienced symptoms such as exhaustion, feelings of dehydration, frequent urination and a foggy mind. Additionally, diabetes weakens the immune system, which means that diabetics are sicker for longer and their symptoms are often magnified.
“[Having diabetes is] a full-time job, you’re doing basically what your organ should be doing subconsciously,” Guerrero said. “You’re having to do everything manually.”
Another side effect of diabetes is hypoglycemic episodes. These happen when blood sugar levels drop too low and can result in diabetics passing out, along with an inability to verbalize needs or communicate that they are in an episode. Even more extreme, seizures can occur.
“So, actually, that is one thing I’ve noticed is when I get really, really anxious, sometimes I confuse it with my blood sugar being low. So I have to check my blood sugar and be like, am I anxious right now, or is my blood sugar low? I’ve been anxious a few times … to the point where I have been shaky, and [anxiety and less intense hypoglycemic episodes] have a similar feeling.”
In order to monitor their blood sugar levels, type one diabetics have multiple options. One option is Multiple Daily Injections, or MDIs. This is a system in which syringes are used to inject long-lasting insulin in the evening and shorter timed ones around mealtimes. Another option for type one diabetics is insulin pumps, which last a couple of days and continuously give insulin based on blood sugar levels. To monitor the levels, they use a Continuous Glucose Monitor, or CGM.
“I have a Dexcom CGM, a continuous glucose monitor which is always checking my blood sugar for me,” Hatley said. “It has a small needle that checks my blood sugar and is connected to my phone. I have to change it every ten days. If my CGM isn’t working or I don’t have one I have to prick my finger.”
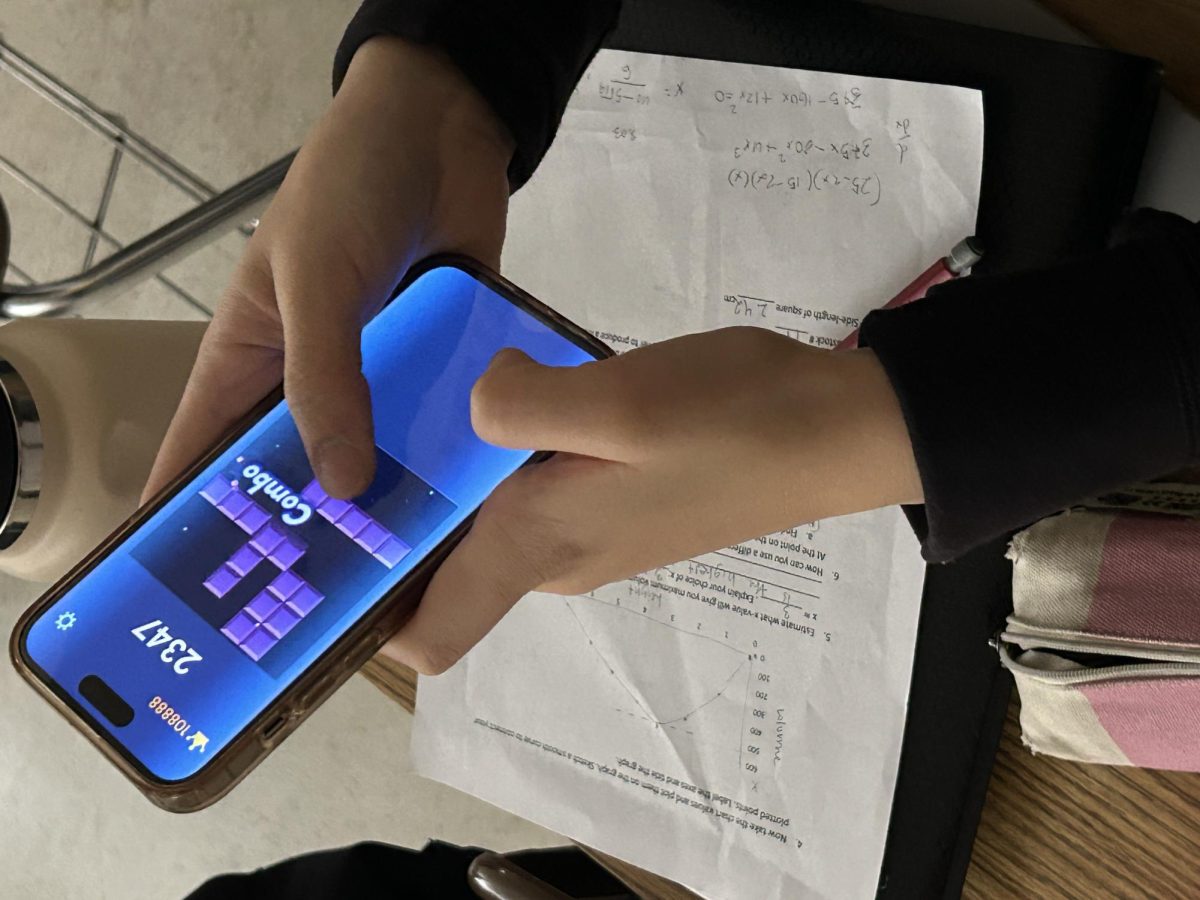
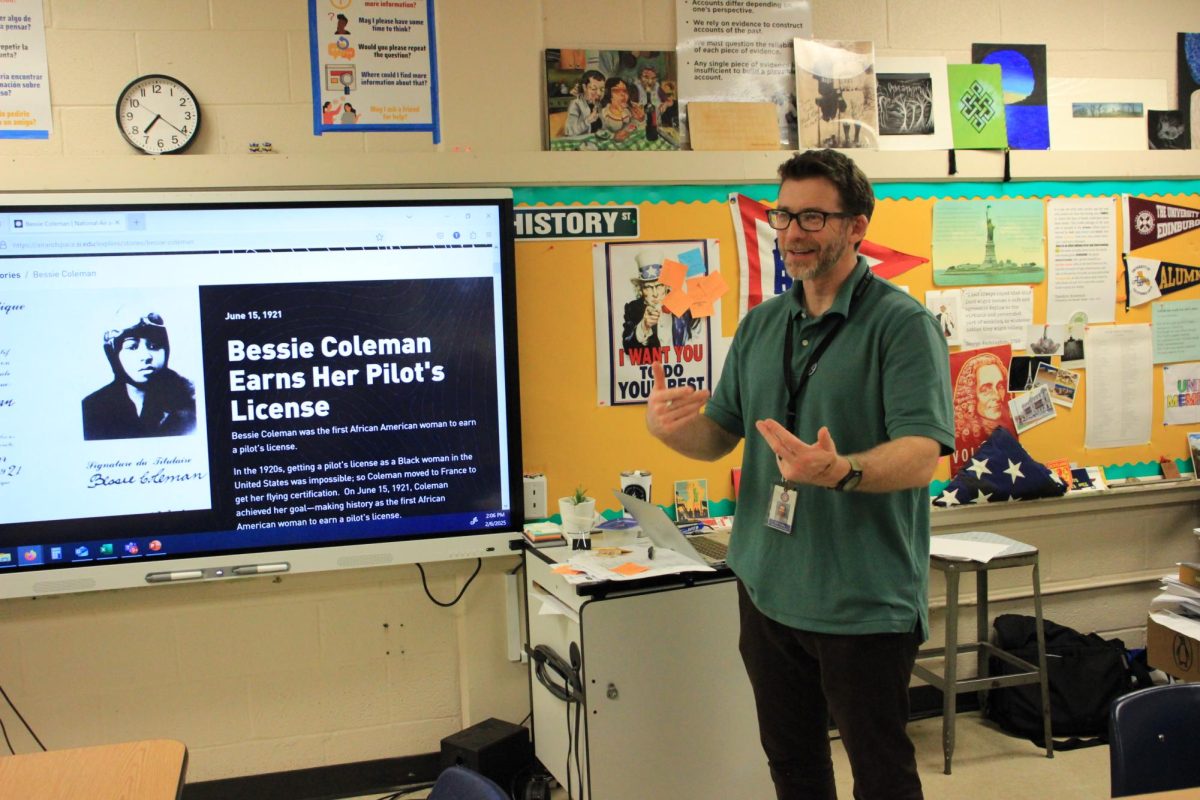
In order to regulate their blood sugar through a CGM, a phone is needed at all times. Consequently, students with diabetes who use CGMs and other electronic tracking devices must be able to communicate these needs to their teachers. Testing can be difficult too, because they have to make sure the school and testing accommodations are secure. Besides the phone, many carry around kits for emergencies and extra food and juice to keep their blood sugar up.
“[Having diabetes definitely can be] a lot of extra baggage, but you can’t opt out of it; it’s not something you can turn off, even if you’re tired,” Guerrero said.
Students with diabetes have to communicate efficiently with their teachers and peers, but there are still a lot of misconceptions surrounding diabetes. For one, many people assume it’s something somebody can control. The assumption that diabetes is caused when they “ate too much sugar,” is not only false but also can be incredibly hurtful.
“There is a little bit of concern because we don’t really have a nurse, and even if we do [and] we try talking to them, they’re like, ‘Ok, well, if something does happen, we’re just gonna call 911,’” Guerrero said. “[But in reality,] it might be too late by the time they get here if something does happen.”
Therefore, not only can chronic illnesses like diabetes be physically exhausting, they can be emotionally exhausting too. Guerrero, Larsen and Hatley all have struggles with being diagnosed with type one diabetes and have to live with the side effects of that, whether it’s symptoms or the stress that follows them.
“Not a lot of people realize how mentally taxing having a chronic illness can be,” Larsen said.
“If it’s diabetes, or if it’s something else, I think it’s important for people to realize that … it can just make you frustrated with yourself even. So, I think it’s important for people with chronic illnesses when they’re feeling that way to reach out to somebody. If either, it’s a friend, family member, or somebody else who has the same thing going on.”